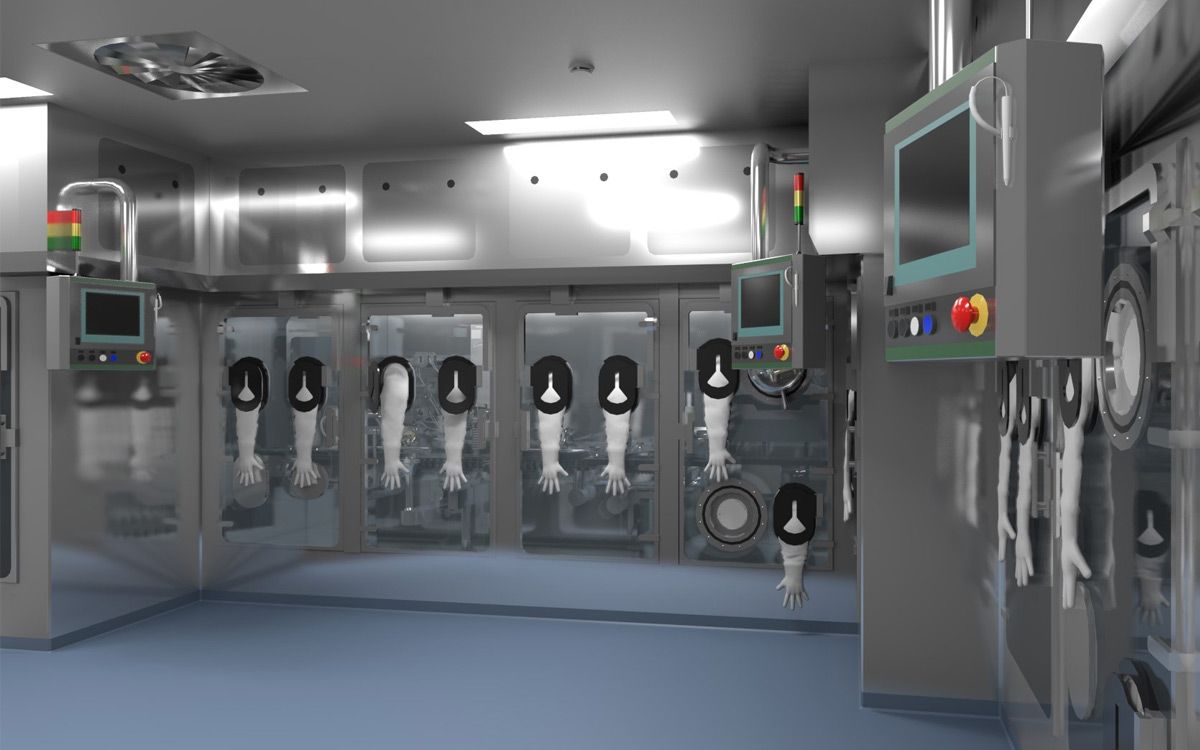
Navigating the selection of a pharmaceutical isolator for aseptic processing?
- 1. Airtightness of the Isolator Chamber:
- 2. Isolator Material Selection:
- 3. Product Compatibility:
- 4. Environmental Monitoring Strategies:
- 5. Glove Integrity Testing:
- 6. Particle Control Measures:
- 7. Bio-decontamination Methods:
- 8. Material Transfer Considerations:
- 9. Equipment Selection for Isolator Use:
- 10. Airflow Design and Considerations:
- Conclusion
This article unpacks 10 crucial considerations. From airtightness and material compatibility to particle control, decontamination methods, and airflow design, this guide empowers you to make informed decisions for efficient and compliant aseptic operations.
1. Airtightness of the Isolator Chamber:
- Ensures operator safety during decontamination by containing cleaning solutions.
- Minimizes particle ingress and product contamination.
- Provides enhanced containment for hazardous materials.
- Achieved through hermetic sealing and advanced sealing technologies like inflatable door seals.

See more: Compounding Aseptic Isolators
2. Isolator Material Selection:
- Low-carbon stainless steel with a polished surface is preferred due to its cleanability and compatibility with decontamination solutions.
- Glass is another common material for its similar properties.
- Air handling system materials should also be compatible, avoiding painted steel or other unsuitable options.
3. Product Compatibility:
- Certain products, like those containing proteins, might be sensitive to decontamination solutions.
- Mitigate this by minimizing absorbent materials in the isolator and potentially modifying sensitive materials.
- Establish acceptable residual concentration levels of cleaning agents through isolator testing.

See more: Cleanroom Isolators Aseptic Processing
4. Environmental Monitoring Strategies:
- Design the isolator and operation procedures with appropriate monitoring points and frequencies in mind.
- Utilize isokinetic funnels for minimal disruption to airflow during air sampling.
- Consider both automated and manual sampling methods (settling plates, swabs) with transfer isolators for manual sampling.
5. Glove Integrity Testing:
- Both visual and automated inspection methods are required by the FDA for isolator gloves.
- Visual inspection requires trained personnel and consideration of access during installation.
- Automated testing might require glove removal, neglecting connections and sleeves.
- On-site inspection takes longer but allows testing during isolator operation.

See more: Isolator Aseptic Processing in the Pharmaceutical Industry
6. Particle Control Measures:
- Maintain a positive differential pressure to prevent particle ingress from the environment.
- Design isolator components (equipment, parts, piping) and disposables to minimize particle generation.
- Thoroughly clean objects entering the isolator and the isolator itself before decontamination.
- Monitor processes occurring within the isolator, especially near open working areas.

7. Bio-decontamination Methods:
- Two main types of bio-decontamination systems exist: stand-alone and integrated.
- Stand-alone systems are versatile and typically include sanitizing spray, fans, connection tubes, and dehumidification for humidity control.
8. Material Transfer Considerations:
- Material transfer can be a deciding factor for isolator suitability.
- Processes involving large volumes, bulky equipment, or non-sterile materials might not be ideal for isolators.
- Utilize sterile pass boxes and transfer port systems for aseptic material transfers.
- Batch or continuous transfer methods can be employed depending on process needs.

9. Equipment Selection for Isolator Use:
- Equipment within the isolator must be easily cleanable, decontaminable, and have minimal seams for optimal hygiene.
- Prioritize high-quality, reliable equipment to minimize disruptions during operation.
- Ensure equipment is accessible through glove ports for adjustments and maintenance after decontamination.
10. Airflow Design and Considerations:
- Unidirectional airflow is crucial for open isolators, especially during transfers.
- Sealed isolators can have unidirectional, turbulent, or non-directional airflow depending on the process.
- Airflow plays a vital role during decontamination, ensuring proper distribution of sanitizing agents, temperature control, and ventilation.
- Large isolators might require dedicated HVAC systems for adequate airflow and distribution.
Conclusion
Selecting a suitable pharmaceutical isolator requires careful consideration of various factors. Collaborating with an experienced isolator supplier can help implement modern features and ensure efficient operation tailored to your specific needs.